The brain is the most complex part of the human body, weighing only 3-lbs., it is also the most fragile organ in the body. It houses the chemicals and cells that are necessary to breathe, move, think and every other aspect of living which you can imagine.
Traumatic brain injuries have been deemed the “signature injury” in post-9/11 veterans. Studies also show that a majority of those who’ve served in Iraq, Afghanistan and other locations during the Global War on Terror suffer five-times the multitude of brain injuries than those during previous armed conflicts. This is a direct correlation from the increased use of homemade explosive devices (IEDs, VBIEDs, etc.) and guerilla warfare tactics utilized by combatants; studies do state that roughly 82% of these occur during training. An understanding of the types of improvised devices and their pathophysiological effects and symptoms is necessary to allow proper planning of appropriate treatments and management of the complex poly-trauma that can occur.
BRAIN BREAKDOWN:
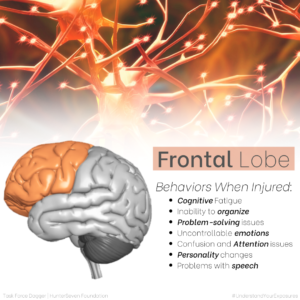
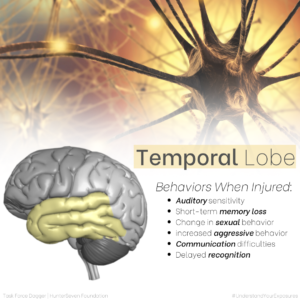
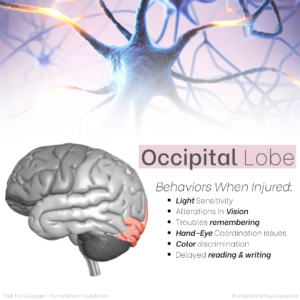
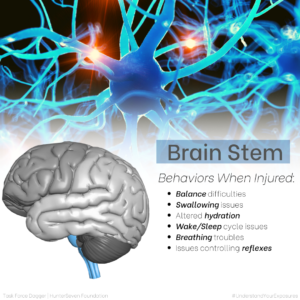
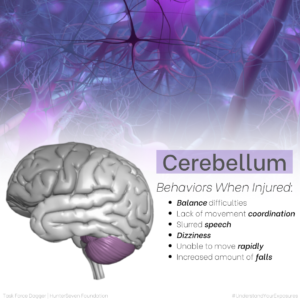
Understanding the major parts and functions of the brain helps both service members and healthcare providers hone into suspected areas of injury. Below we’ve created images that depict the (6) main brain areas (highlighted by color) and the top six behaviors that occur when that part of the brain is injured.
SECONDARY EFFECTS:
Not all brain injuries are the same, how the brain is effected is different in every individual which makes caring for those with a brain injury a very individualized process. Brain injuries can often mimic other conditions such as post-traumatic stress and may go undiagnosed, misdiagnosed or partially diagnosed. Since the brain has a role in every aspect of the human body, an injury to the brain may create a “domino-like” effect on other areas and functions of the body. We’ve noticed brain injury impacts biological, psychological and physiological functioning, exacerbates chronic pain and negatively impacts sleep. This is a cyclical, non-directional, chain of events.
GETTING TREATMENT
Things we can apply here and now that will positively affect our lives long term. Treatment starts with acknowledgment, being your own advocate. Avenues of treatment vary based on your current military status (i.e. Active Duty, Reserve, National Guard, Veteran), your “veteran” status in terms of VHA enrollment, medical status (i.e. medically retired, medically discharged, purple heart, etc.) and your current location (city, state, country).

With brain injuries effecting approximately 430,720 post-9/11 veterans and with an additional unknown number going untreated and unreported, the DoD has made brain health a top priority in creating the Traumatic Brain injury Center of Excellence (TBICoE). The TBICoE is an avenue for both healthcare providers and service members to learn about treatments.
For hands-on assessments and treatments occur in both the in- and out-patient care, the DoD established the National Intrepid Center of Excellence (NICoE) at Walter Reed Medical Center and Intrepid Spirit Centers (ISC) across the country which is a dedicated to TBI care in active duty military. Below are drop-down menu’s for both Intrepid Spirit Centers as well as Brain Injury centers, hyperlinked to contact information for each establishment.
We recommend you schedule your “Separation History and Physical Examination” (SHPE) AT LEAST 90-days prior to leaving military service. Bring with you a copy of your DD-2807-1 “Report of Medical History” and discuss and document every medical issue as this will help you during the VHA disability and healthcare process.

Once a service member is discharged and they transition into “veteran” status they can become eligible to apply for benefits if they haven’t already. More information on applying for VA care can be found here. Veterans can utilize one of the VA’s five-tiered Traumatic Brain Injury Polytrauma System of Care sites based on location and severity of injury. For a full list of all TBI resources the VA offers, please click here.
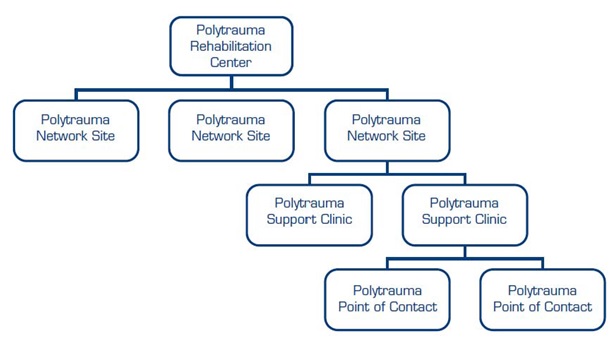
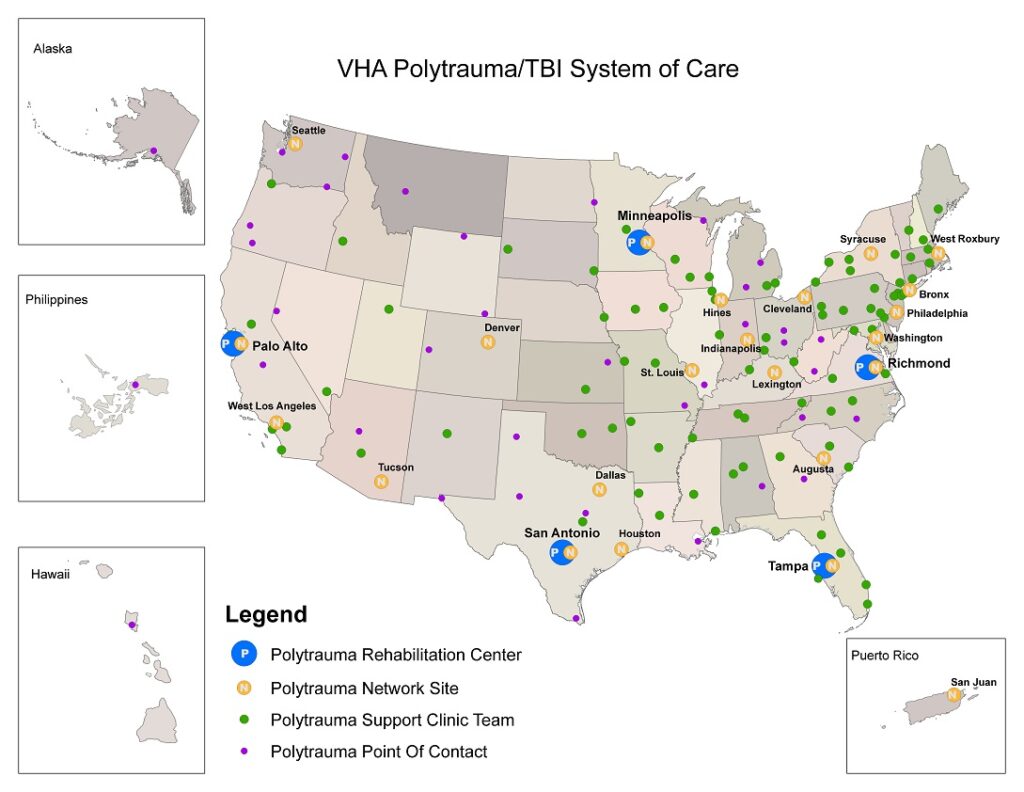
Polytrauma Rehab. Centers (PRCs):
- McGuire VAMC PRC (Richmond, Virginia)
- James Haley VAMC PRC (Tampa, Florida)
- Palo Alto VAMC PRC (Palo Alto, California)
- Minneapolis VAMC PRC (Minneapolis, Minnesota)
- South Texas VHCS PRC (San Antonio, Texas)
Polytrauma Network Sites (PNS):
Polytrauma Network Sites have more locations nationally (23 PNS) and are a step-down from PRC’s for less severe cases. PNS offers continued medical care and rehabilitation services for veterans and service members who are transitioning out to a site closer to their home. Depending on the health care needs, services may be provided inpatient or outpatient.

Given the high operational tempo. in Special Operators, the resources available for traumatic brain injury, polytrauma and dual diagnosis are slightly different and easily accessible for Special Operators both currently on active duty and those with veteran status through the Special Operations Warrior Care Program (SOCOM WCP) located at MacDill Air Force Base, Florida.
The SOCOM WCP assists those who have served in Special Operations as well as enablers of Special Operations organizations with a wide variety of health-related concerns to include wounds, illnesses and injuries. Those looking to obtain support should enroll with SOCOM WCP (can be self-referral or be referred) to begin creating a plan with their personal Recovery Care Coordinator (RCC). Those interested in the SOCOM WCP should email: ussocomcarecoalition@socom.mil or utilize the drop-down list below to find the closest Recovery Care Coordination sites.

SOCOM-Specific TBI and Polytrauma Nonprofit Organizations:
These are just a few of the many special operations focused nonprofit organizations that we’ve worked with over the years that we trust entirely as a key resource in brain health.