February 13, 2023
Exposures to potentially toxic substances occur in our every day lives, everything we do has a potential of being toxic given the appropriate conditions and opportunistic setting. As mentioned in the previous blog post about the serious side effects of inflammation and why it is necessary to manage stress and chronic inflammation to ease the toxic burden your body faces, the same theory applies to heavy metals exposures.
While in military service we are exposed to a variety of chemicals and metals, however, depending on your occupation, duty station, unit assignment, and operational tempo., your risk and rate of exposure differs greatly. Looking at soldiers of an infantry unit as compared to the support element specializing in ordnance or supply within the Arms’ room. Both face exposures, however, the route of exposure (inhalation versus dermal) and dose of the exposure vary. Even when you compare a conventional infantry unit that spends time on outdoor, live-fire ranges and special operations units that operate in closed quarters and confined spaces, those exposures differ as well.
It is important to understand the foundation of toxic exposures to convey the purpose of exposure prevention, risk reduction, symptoms and associated medical conditions as well as next steps to take in regaining control of your health. Below, we’ll cover three topic areas, first being what the academic literature and research says about heavy metals exposures, second, the known health effects, related symptoms and how the body reacts, and lastly, ways to lessen the exposure load and resources for more in-depth screening and treatments through licensed providers.
How are we exposed to heavy metals and toxins while in uniform?
The most obvious route of heavy metals exposures is through firearms and related weapons systems. Now, before we catch hell, we want to make one thing clear. We are NOT asking you to give up your firearms or discontinue shooting to mitigate the risk of exposures. Frankly, our team combined probably has more firepower than the local State Police. We want you to take preventive action to reduce exposures risk. Now, on to what the literature says:
It is no doubt that gunshot fumes are cytotoxic (dangerous to your cells), and have the capability to induce DNA-damage in vital organ systems due to a complex mixture of gases and aerosols consisting of small particulates and liquids (I can still taste the familiarity of CLP). Shooting small arms generates fumes that contain a substantial number of micron-sized nanoparticles that become airborne and suspended in the air. The toxicity of those particles varies based on indoor vs. outdoor shooting, type of firearm being used, caliber and components of bullet being fired. One study in particular reviewed 5.56 x 45 NATO rounds in both soft-lead core and steel core, fired from an HK416 rifle. Something to note about the HK416 rifle is it’s a piston-driven system which may propel a larger amount of gas forward.
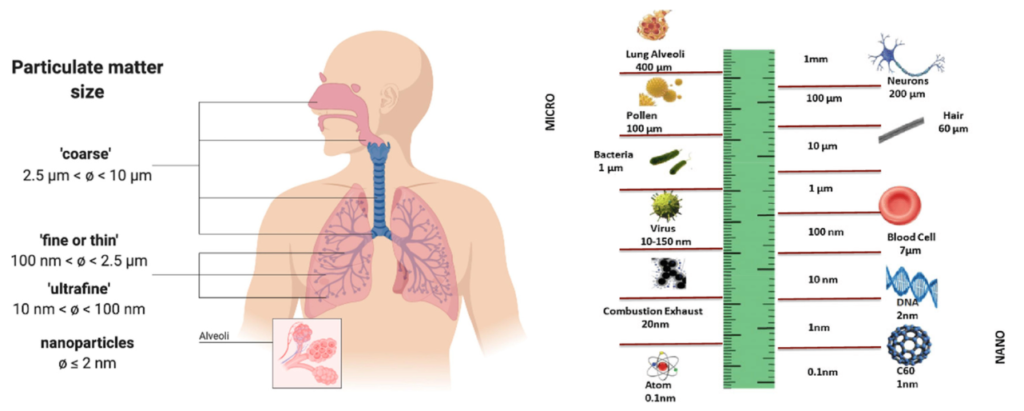
This study looked at the number of particulates and lung-cell viability after variations of 5.56 x 45 rounds had been fired. Ninety percent of particulates generated was (on average) 30nm (nanometers) in diameter, making them capable of mutagenic, and cell-altering potential. For reference, an atom is 0.1nm, and a virus ranges between 10-150nm, while combustion exhaust equals approximately 20-40nm in size. As seen in the picture below, once smaller particulates are able to enter the lower respiratory tract, the gas exchange in the alveoli and capillaries can allow for that particulate to readily enter the bloodstream.
The exposures extend beyond Lead (Pb), and include Copper (Cu) and Zinc (Zn) as well. In addition to the metals, the fumes that are produced from the ignition of the primer and the propellants from the friction between the bullet and barrel offer a unique airborne mixture. Samples found unique gases including hydrogen chloride, ammonia, hydrogen cyanide, and carbon monoxide. And the more rapid the firing, the more gas propulsion was identified.
After the highest levels of 5.56 x 45 gunfire exposure in an indoor setting led to reduced lung cell viability within 24 hours of approximately 40%. This was noted in steel core munitions at just 10 rounds fired (see chart). Thankfully, most human cells and tissues are resilient, and can be easily regenerated and ‘bounce-back’ to normal functioning levels within a week following the acute (short-term) exposures. Most symptoms will occur up to 24 hours following the exposure and mimic flu-like symptoms (we’ll cover this below), but dissipate shortly after. Why is this? Well, this specific study shows that 75% of Cu and Zn particulates, 60% of soot, and 95% of Pb particulates deposit into the lung through inhalation and settle into the thoracic lung region.
Feeling like you have the flu following a day at the Range? Here is why: “Metal Fume Fever”
Metal fume fever is the grouped terminology for a set of symptoms see in those exposed to levels of heavy metal fumes on a regular basis, coined first in the welding profession. Symptoms occurring and reported reflect those which are considered inclusive of “Gulf War Syndrome” and most frequently include:
- Fever
- Unspecific pain, body aches
- Nausea
- Headache
- Cough/wheezing
- Fatigue
- Shortness of breath
As mentioned, these symptoms are usually self-limiting and reduce within a few days of exposure avoidance. But both the 5.56 x 45 munitions (steel and lead core) induced temporary but prominent findings in blood samples identified increased CRP (C-Reactive Protein – see “Inflammation” post) and carboxyhemoglobin which is why we feel light-headed or have headaches following range day.
But what if those exposures cannot be prevented, for example, if you are in a special operations environment and high operational tempo requires training consistent with indoor shoot houses and high numbers of rounds placed on target (because let’s be honest, no one wants to count left over rounds). A well-known Green Beret had experienced this firsthand. Army MSG Geoff Dardia began working as a Special Forces training instructor in 2009, teaching high-intensity courses to fellow Green Berets at Fort Bragg. In a single six-week course, each student would fire roughly 150,000 rounds. MSG Dardia would teach 16 of these courses in just a three-year period. He began having debilitating symptoms including those mentioned above, and it wasn’t until he deployed overseas that he actually began feeling… better?
MSG Dardia was concerned about his symptoms after he returned home, but was more concerned about losing his job on the teams and as an instructor based on those symptoms of unknown cause. He met fellow Green Beret, Stephen Hopkins, who faced similar symptoms. The two became the first active duty service members to be tested and treated at Mount Sinai for chronic lead and toxic metals exposures.

This isn’t a knock to special operations or the Department of Defense, just as any job and work setting; exposures happen. More so, these issues are difficult to identify because the symptoms are ill-defined and can be related to a range of medical conditions post-9/11 military veterans face, including traumatic brain injuries, mental health concerns, autoimmune conditions, etc. The differentiated source is in the blood within days to weeks (less than 25 days) following exposures.
Why 25 days?
The “half-life” (the amount of substance in body reduced by half) of Lead in the bloodstream is roughly 25-30 days. Meaning, we may not be able to detect the accurate amount of one’s exposure in the blood if we do not test within that window as the Lead moves into the tissues and more importantly, the bone.
So where does the lead that enters the body go? On average, 70% is excreted from, and leaves the body. The other 30% that is not excreted is exchanged primarily among three bodily compartments:
- Blood,
- Mineralizing tissues (bone and teeth), and
- Soft tissues (liver, kidneys, lungs, brain, spleen, muscles and heart tissues).
The route of exposure, whether inhaled (like while actively shooting), ingested (through eating and drinking), or absorption (dermal skin contact). Inorganic Lead (munitions) is not metabolized in the liver, whereas organic Lead compounds like those in leaded gasoline (such as in Iraq, Afghanistan, etc.) are solely metabolized in the liver.
Once Lead moves into the tissues, and eventually finds its ‘forever home’ in the bones and teeth, it has the ability to remain resident for 30+ years, making this difficult for clinical care providers to identify and test. There are a few situations where the bone-to-blood mobilization of Lead occurs, those situations include broken bones, hyperthyroidism, Calcium deficiencies, and physiological stress (such as that deployment-related stress we’ve all experienced). Additionally, female service members and veterans face this risk during pregnancy and lactation as well as menopause.
What do Lead and other heavy metals exposures do to the body?
Lead exposures have a wide variety of adverse health outcomes in numerous organ systems. One strong correlation is the inverse relationship of Vitamin D deficiencies and Lead exposures. An underlying issue we see quite often in post-9/11 military members and veterans. Exposures can increase risk and rate of male infertility, thyroid function, irritable bowel syndrome (IBS) and gastrointestinal pain, cardiac concerns (high blood pressure), neurological dysfunction (confusion, fatigue, etc.), respiratory conditions such as bronchitis, asthma, scarring, and has the potential to cause cancer (deemed “probable human carcinogen”).
Now the Important stuff: Ways to rid the body of Lead and other heavy metal toxins:
First and foremost, the best treatment is prevention. But for those who have been exposed recently or chronically, we have gathered some resources for you all. DISCLAIMER: This should not be considered medical advice, and you should explicitly speak with your healthcare team prior to attempting any detoxification or chelation program.
Detoxification of the body is systemic, meaning it is an all-organs systems approach. It is also important to have sustainability – meaning you sustain this lifestyle by beginning slow and working up. The more heavy your exposures have been or currently are, the more slow you’ll want to go. I mention this as I had told Dr. Gabrielle Lyon that I was cutting 90% of carbohydrates out of my diet on Day 1. She advised me not to as I’d feel terrible. Of course, being stubborn I did it any way. From 800g of carbohydrates to 80g a day. For a week I thought I was dying, it felt like I had the flu. Case in point: Start slow to sustain.
Success Starts with SLEEP. It is the core component of health and wellness. Sleep is when your body does its most active ‘detox‘ beginning with your brain. When our medical provider team paired with veteran-owned supplement company Bravo Actual, our intention was to create a natural, non-addictive sleep aid that took the key fundamentals of recovery to address this exact problem. We all work in high-stress environments, high-stress jobs. It is critical to be able to ‘turn off’ after your shift, thankfully our collaboration through “RACK OUT” has made quite a difference.
We are what we EAT, diet plays a large roll in passively assisting the body in detoxification of recent, short-term exposures to toxins. While we cannot guarantee that everyone who eats these foods will feel better instantly, as no one human genome is the same or reacts in a similar manner. But this is a great starting point. We also included a few books down below that we highly recommend giving a read!
- Selenium (Brazil nuts, eggs, spinach)
- Vitamin E (Red peppers, spinach, almonds)
- Vitamin C (Kakadu plums, oranges, pineapple)
- DHA (Omega-3 Fatty Acids)
- Glutathione (Spinach, avocados, asparagus)
- Dandelion tea
- Fresh Parsley
- Fresh Cilantro
- Broccoli sprouts
- Turmeric
- Ginger
- Chia Seeds
- Chlorella pyrenoidosa – broken cell wall type
This a WHOLE BODY change, a multi-systems approach. Meaning sleep and diet are important, but what about the other organs that help detox the body? We’ve included some of our favorite, safe, alternatives below:
- Lungs: Your lungs give you life, if you cannot breathe, you cannot survive. Clean air is key. It isn’t a bad idea to grab some plants while you are at it. Plants help oxygenate the home, unless you are on chemotherapy or immunocompromised – buy more indoor plants.
- Skin: What goes ON your skin, goes IN your skin. And showering with warm, hot water allows for your pores to open up and absorb many toxins unknowingly which passively enter the bloodstream. Some hidden exposures include bug spray, sunscreen, and daily hygiene products. We suggest using natural, skin-safe, non-toxic products.
- Kidneys: Drink * More * (purified) Water. Every morning grab some room temperature, filtrated water. Not water from a plastic water bottle that has been sitting on the counter for a week, but fresh water. Squeeze some fresh lemon juice in there, 20oz. to start the day. But throughout the day stay hydrated. At least 2L daily.
- Liver: The liver is responsible for hundreds of daily functions occurring every minute of every day. Our liver is also one of the most abused organs in our body. Many of these toxins we are exposed to can cause liver damage, as is why many of us who have served experience NAFLD – “non-alcoholic fatty liver disease”. Thankfully, the liver is resilient. Once the toxin is removed, the liver can heal. Switch over to healthy oils which may aid in this recovery process: Avocado Oil, Coconut Oil, etc.
- Lymphatic system: kick start your immunity first thing in the morning by moving. Simply moving. A brisk 15-minute walk, jumping jacks, something to get your lymph circulating. This also helps kick-start glucose consumption which is a necessity for those battling cancer. Another option could be a minute-long ice bath or ice shower to wake you up.






If you are, what seems like the “point of no return” and you’d like assistance in clearing these toxins professionally, we can recommend some healthcare providers who have worked closely with the military and veteran community.
- CHRIS MCKINLEY, Physicians Assistant, former Navy SEAL, Trinity Wellness Center
- GABRIELLE LYON, Functional Medicine Provider, SOF Provider, Owner of Lyon Institute
- BRYAN STEPANENKO, Medical Doctor, former Army Provider, Lead Physician at the Lyon Institute
- KEVIN LACZ, Physicians Assistant, former Navy SEAL, Lifestyle and Performance Medicine
- MARK GORDON, Medical Doctor, Military Medical care, Millennium Health Center
